Infertility in Females
Infertility in Females
Several factors can contribute to female infertility including age, anovulation, tubal, and cervical-uterine issues. 1 in 8 couples have trouble conceiving. At Precision IVF you are not alone and we are here to help. Women under the age of 35 who have been trying to get pregnant for a year and women over the age of 35 who have been attempting to conceive for 6 months without success are recommended to consult specialists. Women with more than two consecutive miscarriages could be experiencing fertility problems.
Lifestyle Factors
Some of our everyday choices can affect our fertility. It is crucial to practice proper nutrition as well as routine exercise to help prepare your body for a healthy pregnancy. Overweight women with a body mass index (BMI) higher than 29 and underweight women with a BMI less than 19 are potentially at higher risk for experiencing infertility.
When trying to conceive, avoid unhealthy habits such as smoking, drinking alcohol, and recreational drug abuse. Changing these habits and optimizing your health will not only improve your chances of conceiving but will also allow for a healthy baby and you.
Factors Affecting Female Infertility
While there are a multitude of diagnoses, we will outline the most commonly seen causes:
Tubal factor:
Open (patent) and functioning fallopian tubes are necessary for pregnancy to occur. Tubal disease is a disorder in which the fallopian tubes are blocked or damaged. This is usually caused by a history of previous pelvic infections, previous pelvic-abdominal surgery, or endometriosis. Tubal blockage accounts for 35 percent of female infertility. The test that is typically performed to assess tubal patency is a hysterosalpingogram (HSG), which is an X-ray picture of the pelvis. A thin tube-like instrument passes into the cervix, then an X-ray dye is injected into the uterus. As the dye enters the uterus and fallopian tubes, an assessment can be done on the uterine and fallopian tube anatomy.
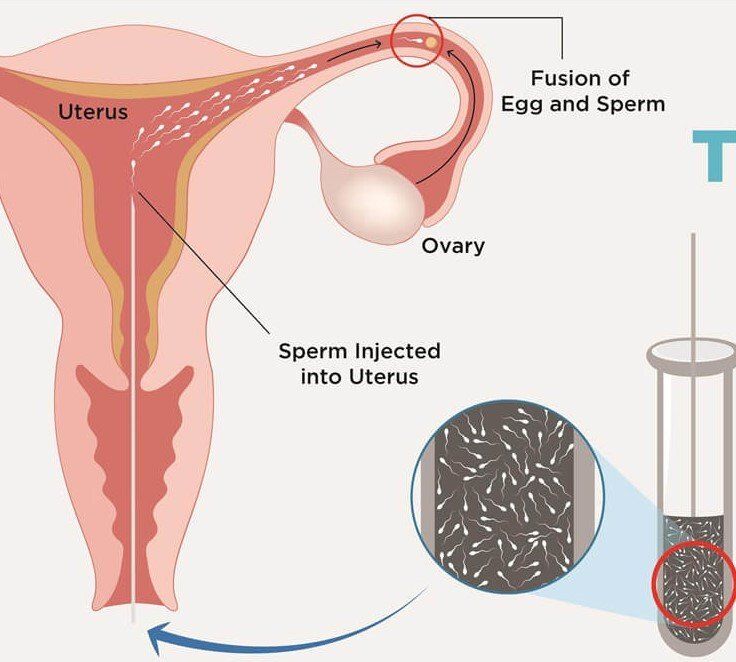
Cervico-uterine issues: The cervix is located in the lower part of the uterus. Conditions of the cervix can affect fertility, however, they are rarely the sole cause of infertility. The following conditions can contribute to cervical factors: abnormal pap smear(s), prior cervical biopsies, cervical surgery (cone biopsy) and “freezing” and/or laser treatment of the cervix. Cervical problems are generally treated with antibiotics, fertility medications or by intrauterine inseminations (IUI).
The uterus (womb) is where the fertilized egg implants and develops. Uterine abnormalities can account for 20 percent of female infertility and includes:
- Uterine scar tissue from previous uterine surgery or miscarriage (Asherman’s Syndrome)
- Polyps (usually benign growth of the endometrial lining)
- Uterine fibroids
- Abnormally shaped uterine cavity
Problems within the uterus may interfere with implantation of the embryo or may increase the incidence of miscarriage. The test(s) typically performed to assess the uterine cavity include a hysterosalpingogram (HSG) or a saline infusion sonogram, also called a sonohysterogram (SIS or SHG). In SIS, similar to the HSG, a thin tube-like instrument passes into the cervix. A small amount of saline is injected into the uterus under ultrasound guidance to assess the uterine cavity. This is the preferred test for uterine abnormalities. Surgery may be required to further evaluate and possibly correct uterine cavity abnormalities.
Dr. Arya is skilled in treating uterine factors contributing to infertility.
Irregular or no ovulation: Problems with ovulation are a common cause of infertility, accounting for approximately 30 percent of all female infertility cases. In order to conceive, a woman must ovulate (release an egg from the ovary into the fallopian tube). Ovulation is connected to a woman’s menstrual cycle, or period, which takes place every 28 – 35 days depending on the individual. Women who experience a period more than every 35 days are probably ovulating infrequently or not at all. There are many reasons why a woman may not ovulate regularly, many of which are treatable through lifestyle changes or fertility treatment. Some of the common causes of ovulatory problems are polycystic ovarian syndrome (PCOS), thyroid hormone imbalance, high prolactin levels, and higher body weight. Ovulation can be determined through menstrual charting, over-the-counter ovulation predictor kits (OPKs) and blood hormonal (progesterone) testing.
Hormonal imbalances: PCOS is the most common ovulatory disorder representing 85% of all diagnosed ovulatory disorders. Conception can occur with lifestyle modifications and fertility treatment. Female athletes such as marathon runners and gymnasts often experience an ovulatory disorder called hypothalamic amenorrhea. Women experiencing higher levels of prolactin, the hormone that stimulates milk production, often do not ovulate regularly making conception difficult to achieve
Age: Age is a major factor in female fertility. As a woman approaches her mid-30s, her fertility begins to decline. After age 40 there is a sharp decline in conception and an increase in chromosomal abnormalities in eggs. This decline in fertility is because there are fewer eggs in the ovaries and the quality of the eggs diminish as a woman gets older. Not only does age affect a woman’s ability to get pregnant and carry the pregnancy to term, age can also affect the pregnancy itself by increasing the risk of genetic abnormalities in the embryo and miscarriage.
Women in their late 30s and 40s are considered to be of advanced maternal age. While conception is still possible it can be difficult to achieve without the assistance of fertility treatment. Discuss successful treatment options available to help you conceive with Dr. Arya.
Endometriosis : Endometriosis is a diagnosis common among girls and women in their reproductive years. It is a condition in which endometrial tissue (tissue that lines the inside of the uterus) grows outside of the uterus and eventually sheds into the abdominal cavity. Inflammation occurs in the areas where the blood pools, forming scar tissue. When the endometrial tissue forms on other reproductive organs aside from the inside of the uterus, it may interferes with ovulation, tubal transport, and embryo quality. For women with endometriosis, we recommend that you consult a fertility specialist who can discuss an appropriate treatment plan to help you conceive, or determine a plan for future family building if you are not yet ready to have a baby. With proper counseling and care, the chances of getting pregnant with endometriosis are high for most women.
Recurrent miscarriages: Miscarriage is one of the most devastating experiences that can happen to a woman. Approximately two out of every 10 pregnancies may result in a miscarriage. After having one miscarriage, most women go on to have a healthy pregnancy. For some women pregnancy is not a problem, rather maintaining it is a challenge. Women are considered to have recurrent miscarriages when they have two or three miscarriages in a row. About one percent of women have three consecutive miscarriages or more. About 50% of the time we are able to determine the cause of recurrent pregnancy loss.
The causes of recurrent pregnancy loss include:
- Genetic-chromosomal defects
- Age
- Uterine abnormalities
- Incompetent cervix
- Hormonal defects
- Autoimmune disorders
- Clotting disorders
Treatments vary depending on the cause of recurrent pregnancy loss including hormonal-anticoagulant medications, surgery, IVF, and pre-implantation genetic screening. Due to the nature of recurrent pregnancy loss, many couples may not immediately seek help to treat this condition as they are able to conceive. However, it’s important that a physician help address the underlying cause of the miscarriages. Some couples experience infertility as both delayed conception and recurrent loss.