A Step-by-Step Guide to Intrauterine Insemination (IUI)

What is IUI?
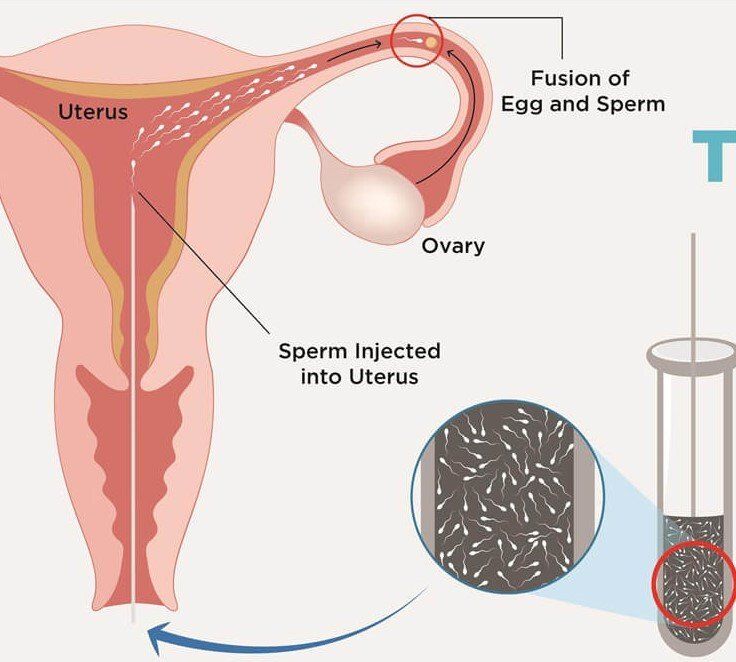
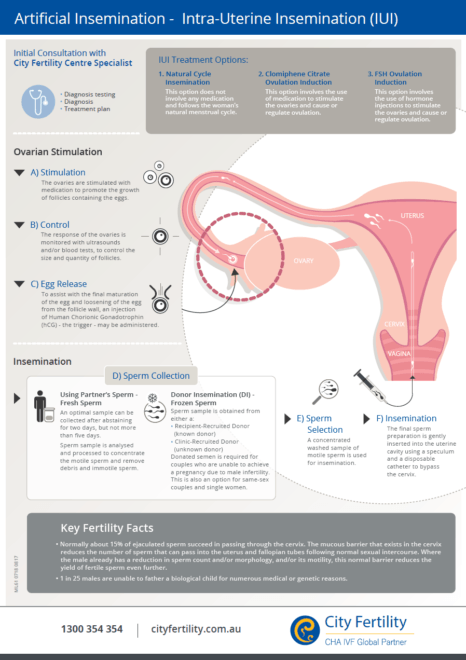
An IUI is also known as artificial insemination in which sperm is placed directly into your uterine cavity near the time of ovulation. This procedure can be performed either with your partner’s sperm or with donor sperm.
How does the IUI procedure work?
IUI is considered the first-line treatment for unexplained infertility, mild endometriosis, or mild male factor infertility.
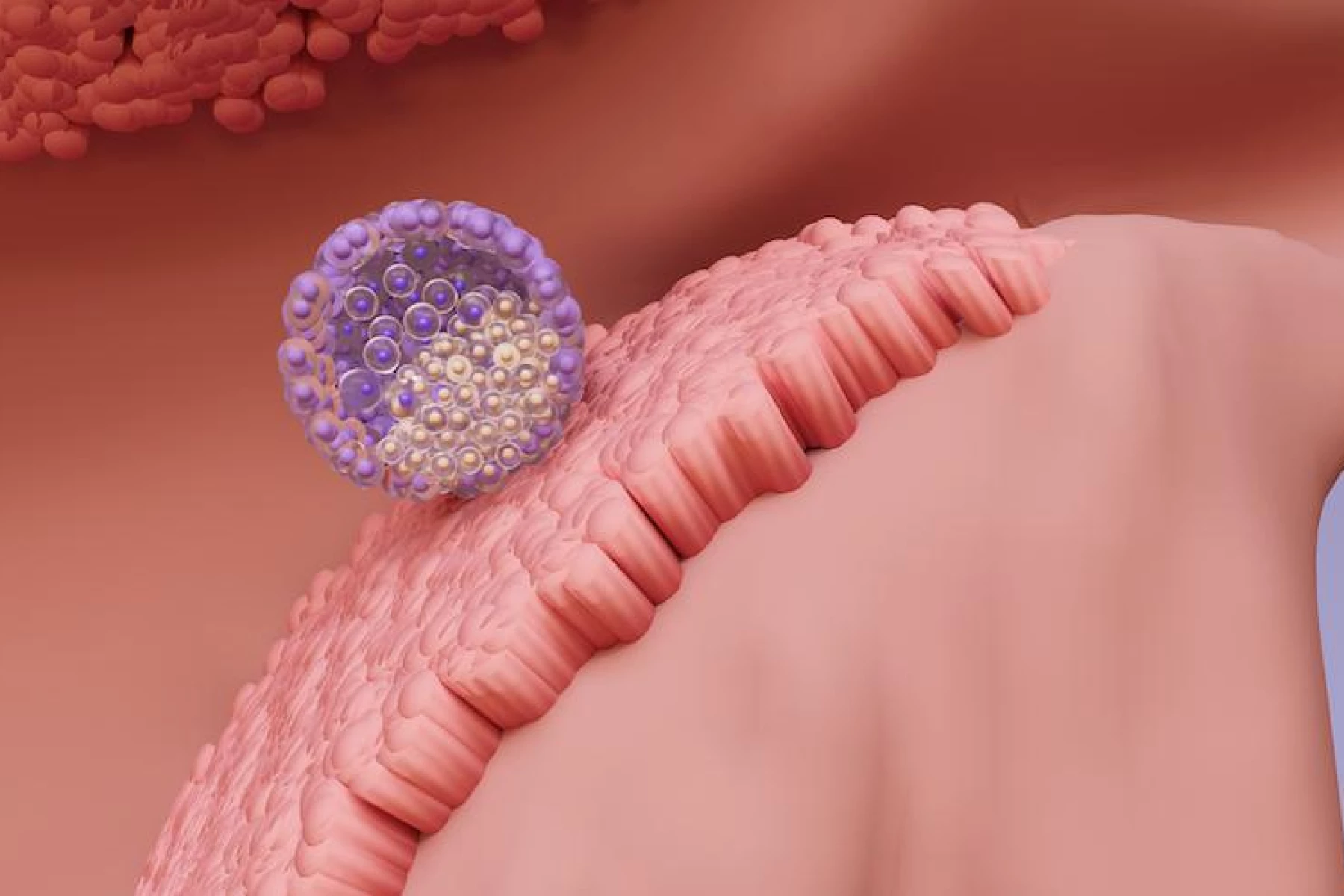
In general, IUI does two things differently than natural attempt to conceive: ovary stimulating medication (taken before the “HCG trigger injection”) help stimulate the growth of follicles (each follicle has an egg in it), making a woman more fertile than she would be in a natural cycle (without the medication). 2nd, the injection of sperm that is placed inside the uterine cavity, avoiding having to swim through the cervical opening and into the uterus on its own, allowing it to meet the egg more easily and at higher concentration. This is especially useful when the sperm count is low or the sperm do not move well. IUI bypasses the vagina and cervix, hence overcoming incompatibility between sperm and cervical mucus if there is any.
During the procedure, the male partner will be asked to provide a semen sample about two hours before being scheduled for insemination. This is done by masturbating into a sterile container at the doctor’s office or at home. The semen is “washed” to separate the sperm from the seminal fluid. This must be done before the sperm can be injected into the uterus because the seminal fluid contains substances that can irritate your uterus. Sperm “washing” may also improve the ability of the sperm to fertilize the egg.
The insemination takes only a few minutes. Your fertility specialist will place a speculum inside the vagina, insert a small soft catheter through the cervix into the uterine cavity, and inject the sperm into the uterus. IUI is not a painful procedure, you may experience slight discomfort from speculum placement.
Who are the ideal candidates of IUI?
- Women with unexplained infertility
- Couples where the male partners have minor semen abnormalities or ejaculatory dysfunction
- Couples where male partners froze sperm prior to surgery, travel, or treatment for diseases that may affect his sperm production.
- Women who may not ovulate, such as those with PCOS, or other reasons of anovulation like hypothalamic amenorrhea.
- Anyone who needs donor sperm, such as LGBTQA+ couples, heterosexual couples with severe male factor who are not able to do an IVF cycle, or single women by choice
How much does IUI cost?
IUI is much less expensive than
in vitro fertilization (IVF) and is many times covered by commercial insurances, making it a much more accessible and affordable option. IUI is also much less involved and invasive compared to IVF. The average cost of an IUI cycle is around $800.
What preparation do you need to do for an IUI?
Before the IUI procedure, you’ll need to do some testing to ensure that IUI is the right treatment for you. It involves the following fertility test, all these can be done in 1 visit prior to IUI:
- Ovarian reserve test- by antral follicle count (AFC) done using ultrasound and/or a blood test called anti-Mullerian hormone (AMH) level.
- Your doctor may suggest you to do genetic blood work to find out whether you’re a carrier for any particular genetic mutation.
- You’ll have a hysterosalpingogram (HSG) to ensure your fallopian tubes are patent.
- Semen analysis
Once your basic fertility work up is complete and you are ready to start the IUI treatment cycle, you may receive one of the following medications to grow follicles:
Clomiphene citrate (Clomid) and letrozole (Femara) are oral medications commonly used for IUI cycles. Occasionally your doctor may advise you to take FSH and/or menopur, which are injectable medications for ovarian stimulation. Clomid or Femara are taken orally for 5-7 days typically starting on day 3 of menstrual cycle. In order to appropriately time for this treatment, your ovulation is carefully monitored by midcycle ultrasound and bloodwork. With ultrasound, the uterine lining thickness and follicles are measured, and with blood work, we test estradiol and progesterone. Based on these results, you will be advised to get an HCG injection (“trigger shot”) to help in ovulation and the timing of the IUI procedure. IUI is typically scheduled 1-2 days after ovulation begins. For IUI to be effective, it must be performed before or within 24 hours of ovulation, or the egg is no longer fertilizable. The life of an egg is much shorter than the life of the sperm, so there is only a short window of time in which an egg and a sperm can interact and create an embryo. Hence, it is better for the sperm to be in the uterus early rather than late.
Male partner should not ejaculate for 1-2 days before the procedure to maximize sperm count available for IUI. Check with your doctor to see if there are any other recommendations specific to your care.
What are the chances of twins or triplets with IUI?
Because these ovary stimulating medications cause many follicles to mature and ovulate, leading to a higher risk of twins, there are about 10-12 percent chances of twins. Triplet pregnancies are rare with oral medications. Midcycle ultrasound monitoring helps in reducing the risk of multiple pregnancies by knowing how many mature follicles you have. Your doctor may advise you to avoid IUI if you have more than 3 mature follicles on monitoring ultrasound in a particular cycle. The dose of medication can be adjusted to optimize the response and reduce the risk of twin pregnancy.
Will I need multiple IUIs to become pregnant?
The success rate of IUI is typically lower than the IVF cycle. It depends on many factors like ovarian reserve, women age, and sperm concentration. If you don’t become pregnant after an IUI cycle, you may repeat the procedure. Further evaluation or other treatment options such as IVF, may be recommended if a patient does not get pregnant after several cycles.
When you will I know if IUI treatment is successful?
You will know in 2 weeks! if you become pregnant, you will most miss your next period. A blood test will confirm whether or not you are pregnant.
- Sushila Arya, MD MS FACOG