Everything You Need to Know About Infertility
Are you having trouble getting pregnant? Have you tried everything, but it just won't happen? Perhaps you're wondering if you or your partner need to see a doctor. If you're having a hard time conceiving, you're not alone. CDC reports that about 10 percent of American women ages 15-44 (6.9 million) have difficulty getting pregnant and staying pregnant.
The article discusses the causes of infertility in both men and women and different treatment options that can aid in the treatment of infertility.
Overview of Infertility
Infertility is defined as not being able to conceive despite having frequent, unprotected sex for at least a year. There may be issues with you or your partner, or a combination of factors may contribute to it. In general:
- Approximately one-third of cases involve male infertility
- One-third of the cases involve infertility issues for the woman
- In the remaining cases, both the woman and the man are infertile, or no cause can be determined
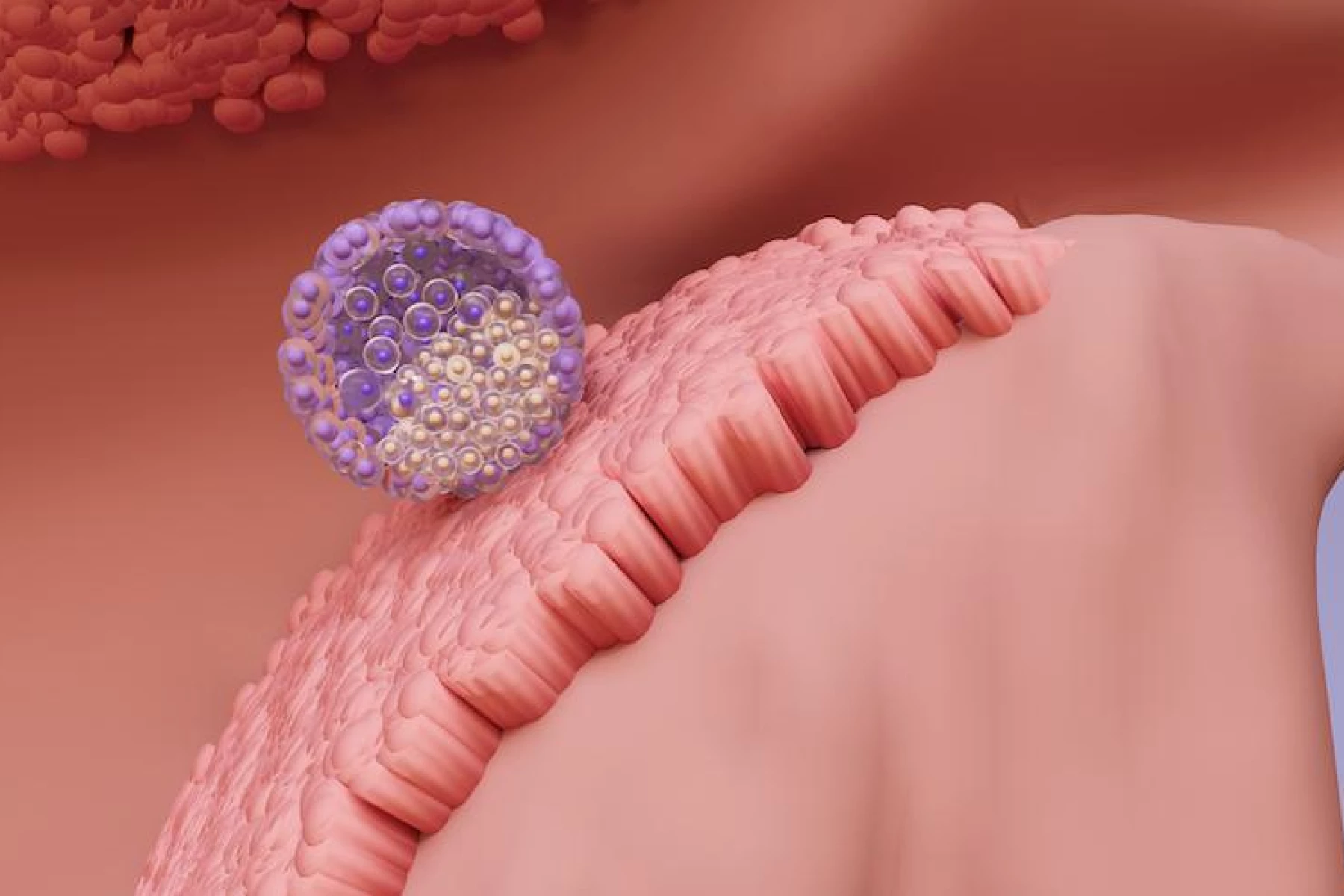
First, a woman's body must release an egg from one of her ovaries (ovulation). Second, the egg must travel through a fallopian tube on its way to the uterus (womb). The next step is for the sperm to join the egg (fertilize it). Lastly, the fertilized egg must implant into the uterus (implantation). A problem with any of these steps can lead to infertility. All steps during ovulation and fertilization must take place correctly to achieve pregnancy.
Risk Factors of Infertility for Both Men and Women
Many factors can affect fertility, both for men and women. Here are the common risk factors for both genders.
- Fertility declines as we age (over age 35 for women or over 40 for men)
- Abuse of substances.
- Alcohol abuse.
- Eating disorders, such as anorexia and bulimia
- Exposure to environmental toxins such as lead
- Excessive exercise.
- Radiation therapy or other cancer treatments
- STDs (sexually transmitted diseases)
- Smoking tobacco and marijuana
- Stress
- Weight issues (obesity or underweight)
Having health problems can also increase the likelihood of infertility. Thus, whenever couples plan to become pregnant, it is wise to talk to a healthcare provider. The doctor can help you address any concerns about conceiving and fertility.
Infertility in Women
All essential parts of a woman's reproductive system must be in working order to get pregnant: the fallopian tubes, the ovaries, and the uterus. Infertility is most often the result of issues with ovulation. Fertilization cannot occur without ovulation. Women who experience painful, irregular, or absent menstrual cycles may indicate that they are not ovulating normally.
What Can Cause Infertility in Women
Apart from the common risk factors among men and women, here are the causes of infertility in women:
- Endometriosis or growth of endometrial tissue outside your uterus prevents the egg from reaching the fallopian tube
- Ovulation disorders and hormonal imbalances interfere with the production and release of eggs. These include hormonal conditions such as polycystic ovary syndrome (PCOS)
- Anomalies of the uterus or cervical region, including abnormalities with the polyps in the uterus and atypical uterine shape
- The effects of certain cancers and chemotherapy, such as reproductive cancers, can negatively affect female fertility.
- Blockage or damage to the Fallopian tube
- Uterine fibroids, or non cancerous/ malignant masses of muscle and tissue on the walls of the uterus.
- High prolactin/ Hyperprolactinemia -Overproduction of prolactin by the pituitary gland can reduce estrogen production and lead to infertility.
- Amenorrhea or the absence of periods caused by extreme physical exertion or deficient body mass index
- Scarring binding organs that can develop from past appendicitis, pelvic infection, endometriosis, and abdominal or pelvic surgery
- Pelvic inflammatory disease (PID)
- Chronic diseases, such as Lupus, arthritis, asthma & hypertension
Diagnosis of Infertility in Women
A fertility physician will begin by taking an in-depth medical and fertility history. Afterward, they will perform a complete physical examination and an ovulation test. A number of these tests following the first two steps can help diagnose or rule out a problem with female fertility:
- Blood testing to check thyroid and hormone levels
- Pelvic exam, including a Pap smear
- Transvaginal ultrasound – For assessing the structure of the uterus, tubes, and ovaries and useful to detect fibroids, polyps in the uterus, fallopian tube obstruction, and ovarian cysts.
- Laparoscopy helps determine if there are problems such as endometriosis, fibroids, or scarring.
- Hysteroscopy: A specialist inserts a tube with a light through the vagina to examine the uterus.
- Hysterosalpingogram (HSG): The test looks for blockages. X-rays are taken during the injection of a dye through the fallopian tubes.
- The saline sonohysterogram (SIS) involves filling the uterus with sterilized salt water and examining it with a transvaginal ultrasound. The uterus is easier to view this way.
Infertility in Men
In cases where male infertility is suspected, the focus is generally on analyzing the semen to determine whether a sperm has successfully met an egg. Part of the male infertility testing includes the number of sperm, their mobility (sperm motility), and their shape.
The presence of slightly abnormal semen does not necessarily indicate infertility. By analyzing semen, an infertility specialist can determine which factors may cause infertility.
What Can Cause Infertility in Men
- Low testosterone (hypogonadism) or low sperm count
- An injury to the testes can lead to a decrease in sperm production.
- History of testicular or prostate disorders
- Varicocele is an enlargement of the veins around a man's testicles, which causes them to overheat and affects the shape and amount of sperm.
- Hormonal imbalance, resulting in insufficient testosterone production
- Ejaculation problems particularly delayed ejaculation or retrograde ejaculation (semen goes back into the bladder)
- Undescended testicle
- Medical conditions such as diabetes, Cystic Fibrosis, and other autoimmune disorders
- A genetic problem with the absence of the main sperm pipeline known as the vas deferens
Diagnosis of Infertility in Men
The first step is for your doctor to take a complete medical history. As part of this process, the doctor will ask about the overall condition of your health, sexual history, and anything else that might affect your fertility. You will also undergo a physical examination where they will examine your genitals for lumps and anomalies. An analysis of the semen will follow. If your doctor feels you require additional testing, they may order the following:
- Semen Analysis to check for sperm problems, including low counts and poor mobility.
- Blood Testing to determine testosterone, hormone, and thyroid levels.
- Ultrasound of the genital area: A scrotal ultrasound detects varicocele and other testicular disorders.
- Genetic testing to check for chromosomal abnormalities.
Medication and Fertility Treatment Options
Being infertile does not mean you will never have a baby. Many couples seek help and can eventually have a child. Making targeted lifestyle changes and modern medical treatments have been proven effective in supporting thousands of couples and individuals on the road to parenthood.
Many treatments are available for both male and female infertility, depending on the underlying cause. The following are some options available for fertility treatment which includes assisted reproductive technology (ART):
- Hormone Therapy
- Surgery which depends on the condition
- Medicines- By taking fertility medication, they can make multiple eggs and increase the probability that sperm and egg will fertilize each other. Examples of drugs are follicle-stimulating hormone, Clomiphene citrate, bromocriptine, and others.
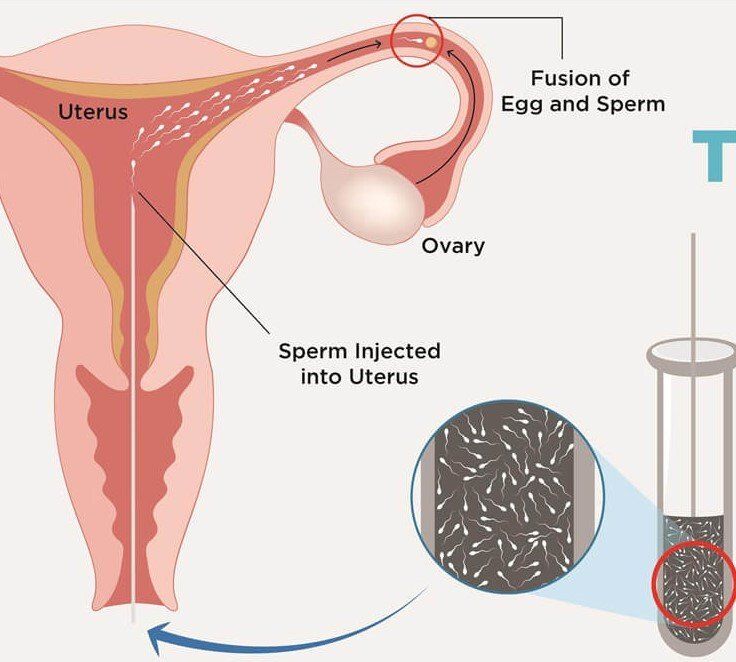
- Intrauterine insemination (IUI) - involves the injection of prepared sperm directly into the uterus during ovulation. The woman is typically given medication first to increase her eggs.
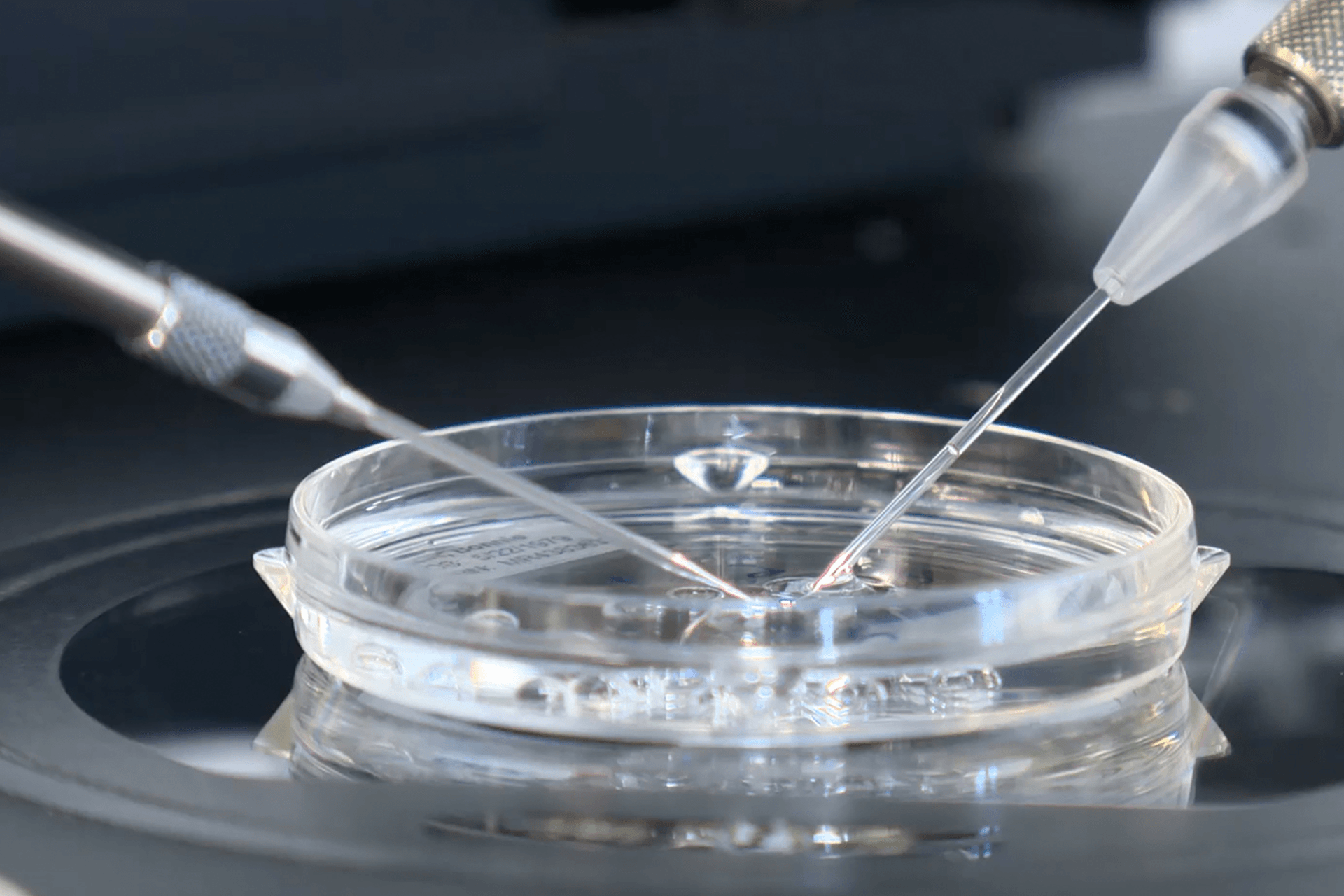
- In-vitro fertilization (IVF)- The doctor mixes sperm and eggs in a test tube in a lab. Once fertilization has taken place, the embryo is moved into the uterus. Embryos that are not transferred can be frozen for use later. In some cases, you may need to undergo more than one round of IVF.
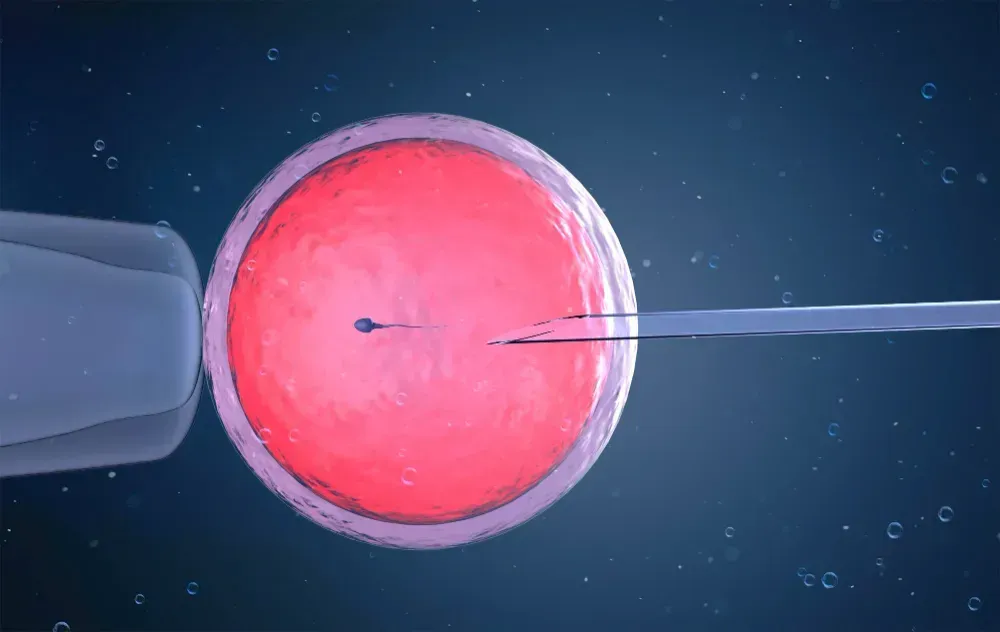
- Intracytoplasmic sperm injection (ICSI) -Involves injection of one sperm into an egg by way of a tiny needle. The fertilized egg is then implanted in the uterus. It is possible to perform ICSI when sperm counts are extremely low or abnormal.
- Zygote intrafallopian transfer (ZIFT) or Tubal Embryo Transfer works similarly to IVF. The process of fertilization takes place in the laboratory. Rather than transferring the embryo to the uterus, it is transferred to the fallopian tube.
- Gamete intrafallopian transfer (GIFT) entails transferring eggs and sperm into the woman's fallopian tubes. In other words, fertilization occurs inside the body of the woman.
- Third-party ART: This is the process by which another person contributes sperm or eggs or plays the role of a gestational surrogate to assist someone or a couple in conceiving a child.
Consult with a Specialist at Precision IVF
Couples over 35 who are trying for six months and under 35 who have been actively trying to conceive for a year should make an appointment with a gynecologist to assess possible female infertility and a urologist to assess male infertility. Depending on your situation, your specialist will make the right recommendation.
We're here to help with infertility in any way we can. Schedule your consultation with Precision IVF today!