Pregnancy & COVID-19 Vaccine FAQ

Pregnancy is one of the most exciting aspects of a woman's life, but pregnancy in a pandemic can be quite challenging. Undoubtedly Covid times had added stress for all and even more to expecting mothers as they worry about their own as well as their unborn child.
As a pregnant woman, there are probably many questions about pregnancy and the pandemic causing you anxiety.
In this article, we hope to provide answers to those questions so you can navigate your pregnancy better. The following section will tackle the most commonly asked Covid-19 vaccine questions related to pregnancy.
Coronavirus and Pregnancy: What You Need to Know
The Centers for Disease Control and Prevention (CDC) released an urgent health advisory urging pregnant women to receive the COVID-19 vaccine. COVID not only leads to worse outcomes for pregnant women than non-pregnant women but also puts their pregnancies at risk.
COVID-19 has led to nearly 22,000 pregnant women hospitalizations throughout the epidemic, and 171 have died as of early October. In comparison with non-pregnant individuals, pregnant or recently pregnant people are more likely to become severely ill from COVID-19. During pregnancy, changes in the body can increase a woman's susceptibility to respiratory viruses like the one that causes COVID-19. This susceptibility may persist postpartum. Current data shows that
- Women with COVID-19 symptoms who are pregnant have a higher risk of needing care in an intensive care unit (ICU) and a ventilator for breathing support. However, overall, the risk of Covid-19 deaths is low for pregnant women.
- Pregnant or recently pregnant women who have certain health conditions, such as diabetes, high blood pressure, or obesity, face a greater risk of serious illness than non-pregnant women with the same health conditions.
- Pregnant Black or Hispanic women are at greater risk for COVID-19-related illnesses and deaths, but not because of biology. Women of color are more likely to experience health, social, and economic inequities that increase their risk of illness. See this CDC page for more information about these inequities.
Frequently Asked Question: COVID-19
Vaccination and Pregnancy
Can pregnant women get the COVID-19 vaccine?
Yes, the COVID-19 vaccines authorized by the Food and Drug Administration (FDA) are suitable and recommended for pregnant women. By vaccinating against COVID-19, you will significantly reduce your risk of becoming seriously ill.
Is the vaccine harmful to my pregnancy?
No. Vaccines do not increase the risk of complications like premature labor, miscarriage, stillbirth, small for gestational age infants, and congenital disabilities.
Can breastfeeding women receive COVID-19 vaccination?
Yes. There is no need to stop breastfeeding before or after vaccination. Recent studies have shown that breastfeeding mothers who have received the COVID-19 mRNA vaccine produce antibodies in their breast milk that might protect their newborns. However, more research is needed to determine what protection these antibodies provide.
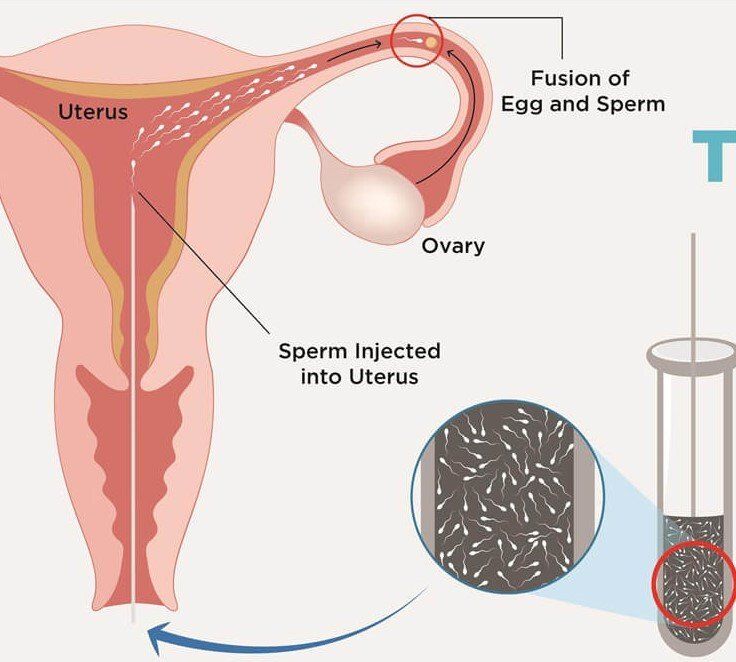
For those trying to conceive, will the vaccine affect fertility?
If you are trying to get pregnant, the vaccine is safe. No evidence exists that COVID-19 vaccines can affect fertility. There's no need to avoid pregnancy before or after vaccination. By getting vaccinated before you conceive, you should be able to protect yourself against COVID-19 during your pregnancy.
What are the side effects of the COVID-19 vaccine on pregnant women?
Women who are pregnant and non-pregnant can experience the same side effects. COVID-19 vaccination may cause the following side effects:
- A bit of pain, swelling, and redness on your arm
- Chills or mild fever
- Fatigue
- Headaches
- Joint pain or muscle pain.
- Mild side effects usually subside in a few days
Severe side effects are extremely rare. When they do appear, they usually appear within 30 minutes of vaccination. You must remain in the observation area for 15-30 minutes post-vaccination. This period is to make sure no serious side effects result from the vaccination.
These severe side effects could include:
- Itching
- Fainting or dizziness
- Vomiting/nausea
- Severe allergic reaction
- shortness of breath, wheezing, or difficulty breathing.
Immediately notify a health worker if you experience these side effects.
Apart from the COVID-19 vaccine, which vaccinations are recommended during pregnancy, and which ones are not?
Generally, it is safe to administer a vaccine that contains killed (inactivated) viruses during pregnancy. A pregnant woman should avoid vaccines that contain live viruses. DTaP vaccine (Tetanus, Diphtheria, Pertussis) and flu vaccines are routinely recommended for pregnant women. It can protect you from infection and make your newborn immune to infection before they get immunized.
This is crucial because flu and whooping cough are especially dangerous to young children. Don't get the influenza vaccine through the nasal spray since it contains live viruses. Moreover, if you're at risk for some infections during pregnancy, your provider may recommend other vaccines, like the hepatitis B vaccine.
What other precautions should I take during pregnancy?
Keep up with the minimum health protocols set by experts to stem the spread of the virus. Here are other precautions you should take:
- Immunization is the best way to prevent getting the virus
- Wearing a mask
- Staying away from crowded areas.
- Regularly wash your hands with soap and water
- Sanitize with an alcohol-based hand rub.
- Keeping a distance from others.
- Maintaining a well-ventilated home.
- Take good respiratory hygiene measures. You should cover your nose and mouth with your elbow or tissue when coughing or sneezing. After using the tissue, dispose of it immediately in a covered bin.
- Maintaining your mental well-being is equally important.
What should I do about my prenatal and postpartum visits?
Visit your healthcare provider for all recommended appointments during and after pregnancy. If you're worried about attending appointments in person due to COVID-19, speak with your healthcare provider about COVID-19 protection measures, or ask about telemedicine options.
Is it safe for me to give birth in a hospital now?
Yes. Birth centers and hospitals are doing everything they can to protect babies and mothers from infection. Hospitals usually isolate COVID-19 patients or those who exhibit symptoms of the disease from other patients.
In some hospitals, delivery rooms are restricted to a certain number of people. You may not be able to bring visitors to the hospital when your baby is born. If they do, they will be screened for Coronavirus symptoms before entering. Consult your physician or ObGyn regarding your birth plan.
Navigate Your Pregnancy Safely!
Emerging strains of COVID-19 are infecting an increasing number of people, so pregnant women, including those who share their home, have to be extra cautious to protect their unborn children from the virus. With Precision IVF, you will have the best support and advice to ensure your pregnancy and your child's safety and well-being. To learn more about our services, call or schedule an appointment online!